
When back pain strikes, it can be unbearable. For most people, a combination of traditional treatments such as rest, anti-inflammatories and pain medications, physical therapy and spinal injections solve the problem. A small percentage of patients will also benefit from back surgery. But what happens when the pain persists even after doctors have tried nearly everything?
For Alexa Alexander, who had already undergone conservative treatments and surgery, some interesting technology and the unending determination of a team of physicians at Baptist Health Miami Neuroscience Institute brought her relief. “After being through excruciating pain, being barely able to walk and then still having numbness, tingling and burning sensations in my thigh, spinal cord stimulation has changed my life,” she says.
(Watch now: Back pain can be unbearable. For Alexa Alexander, after all other treatments had failed, she finally found relief thanks to the experts and advanced technology at Baptist Health Miami Neuroscience Institute. Video by Alcyene de Almeida Rodrigues.)
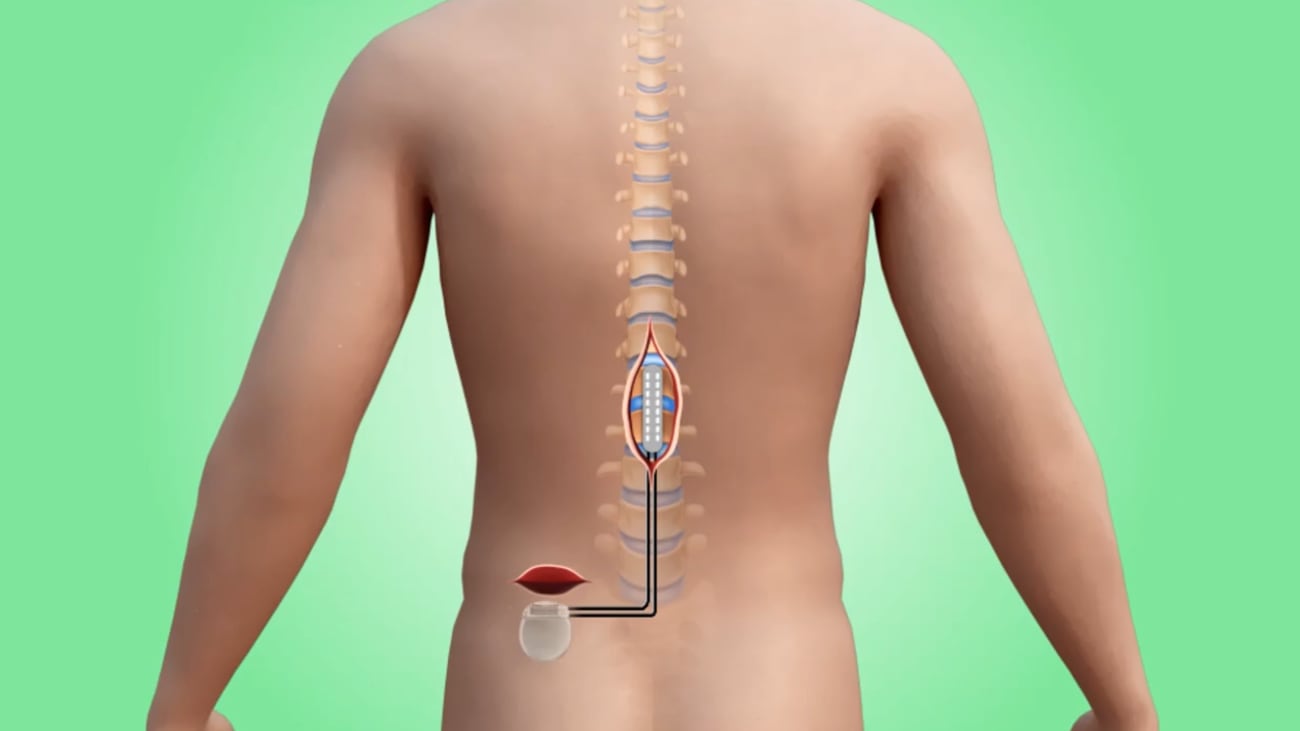
Also known as SCS, spinal cord stimulation involves implanting a small device into the back that emits tiny electrical pulses to the spinal cord to alter the pain signaling process to the brain. “I often describe this to patients as a pacemaker for the spine,” says Akshay Goyal, M.D., a pain management specialist with Miami Neuroscience Institute. “Neuromodulation has existed for a long time, but there’s been a rapid advancement in the technology and the programming abilities in recent years, making it a good option for patients like Alexa.”
Spinal Cord Stimulation Works When Other Options Don’t
SCS is not the initial go-to treatment for patients, however. It’s a choice only after a patient has tried other therapies and been deemed a good candidate for the procedure following a trial run with the device. That was the path taken by Ms. Alexander, whose back pain started in the summer of 2023 when she felt a pop in her back while cleaning her house. After a trip to the ER left her with no answers, she turned to Dr. Goyal. “I could not sleep. I could not sit. The only position that was somewhat comfortable was in my recliner,” she says.
Diagnosed with lumbar radiculopathy from a herniated disc, she had symptoms that included pain in the lower back that radiated to the front of her thigh and down her leg, Dr. Goyal says. Months of physical therapy, pain medications and spinal injections helped the disc problem somewhat, but ultimately, she required surgery.
“The disc was still putting pressure on the most sensitive part of the second lumbar nerve root,” says her neurosurgeon Jason Liounakos, M.D., who specializes in complex and minimally invasive spine surgery at the Institute and works closely with Dr. Goyal. On Feb. 23, 2024, Dr. Liounakos performed a minimally invasive procedure to decompress the nerve and improve her pain.
“Although MRI confirmed she had an appropriate decompression of the nerve, Alexa continued to have pretty severe and disabling pain,” Dr. Liounakos says. “In the absence of any significant structural abnormality, unfortunately there can be chronic irritation of the nerve. That’s where neuromodulation can come in.”
How Spinal Cord Stimulation Works
SCS involves a team approach to ensure the best outcome for the patient, the doctors agree. “What I really like about SCS is that you get to test drive the device before you have it implanted,” says Dr. Goyal, who performed the trial procedure, placing leads into Ms. Alexander’s spine using two small needles. A battery on the outside of the body powers the leads. Daily check-ins with the patient provide feedback on the device’s effectiveness, with the trial considered successful if it cuts pain by at least 50 percent.
“She knew on day two or three that this was going to be beneficial,” Dr. Goyal recalls. “She was able to walk longer distances. She was able to sleep better. And her oral medication use went down.” A week later, she had the trial device removed and discussed a plan for permanent placement.

Akshay Goyal, M.D., a pain management specialist with Baptist Health Miami Neuroscience Institute.
On Jan. 7, 2025, Dr. Liounakos performed the minimally invasive surgery. “It’s a minor surgical procedure with the patient asleep. It involves two small incisions, one in the midline of the lower back where you place the implant and one off to the side for the small battery,” he says. “It typically takes an hour to an hour and a half. There is very little blood loss, the patient is up and walking the same day and goes home the next.”
Using an app on her phone, Ms. Alexander can easily adjust the strength of the pain-zapping signal, as well as its frequency. “There are a lot of different settings,” she says. “I prefer the one called “tingle.” I have it set on a very low power, but it is on all the time. The tingling is pretty much everywhere. I can feel it in my fingertips and in my toes.”
Ms. Alexander compares the feeling to that of a TENS (transcutaneous electrical nerve stimulation) unit, used by many people to relieve muscle and nerve pain. TENS units deliver low-voltage electrical currents to small areas of the body via electrodes placed on the outside of the body.
“The idea behind SCS and TENS is similar,” Dr. Goyal says. “TENS is frequently used in physical therapy and its stimulation is superficial, which is better for muscle pain or myofascial pain. Spinal cord stimulation is deeper in the spine, closer to the nerves.”
An Implantable Device Controls Her Back Pain
The device can remain implanted indefinitely and its battery is rechargeable. “I can feel a little bump where the battery is in my back, but it’s not uncomfortable. And there is a little belt with a plate on it that I put over the battery to charge it,” she explains. “It beeps so that you know it is charging and I can see it on the app.”

Jason Liounakos, M.D., a neurosurgeon with Baptist Health Miami Neuroscience Institute
While SCS is a solution for some patients with back pain, doctors also use it for a widening number of health issues, including diabetic neuropathy, peripheral vascular disease, injuries to the spinal cord and postsurgical pain.
Getting Back to Doing What She Loves
For Ms. Alexander, who turned 50 in February, life is looking bright again. “I enjoy being in my backyard, working on my gardens, making sure all of my orchids are taken care of, being in my pool and playing with my puppies.” Chihuauas Salem and Lyra are excited to have an active dog mom, too, she says. And her husband, Michael, and young adult son, Riley, are happy she is able to participate in family activities and host Sunday family dinners with no pain.
“Without Dr. Goyal and Dr. Liounakos, I don’t know where I’d be today,” says Ms. Alexander, who suffers from some additional health problems including fibromyalgia. “They are awesome, and they would not give up until they got to the bottom of my problem. Having less pain obviously makes things a lot easier in life. I can function better than I could before.”

