

Rupesh Kotecha, M.D.,
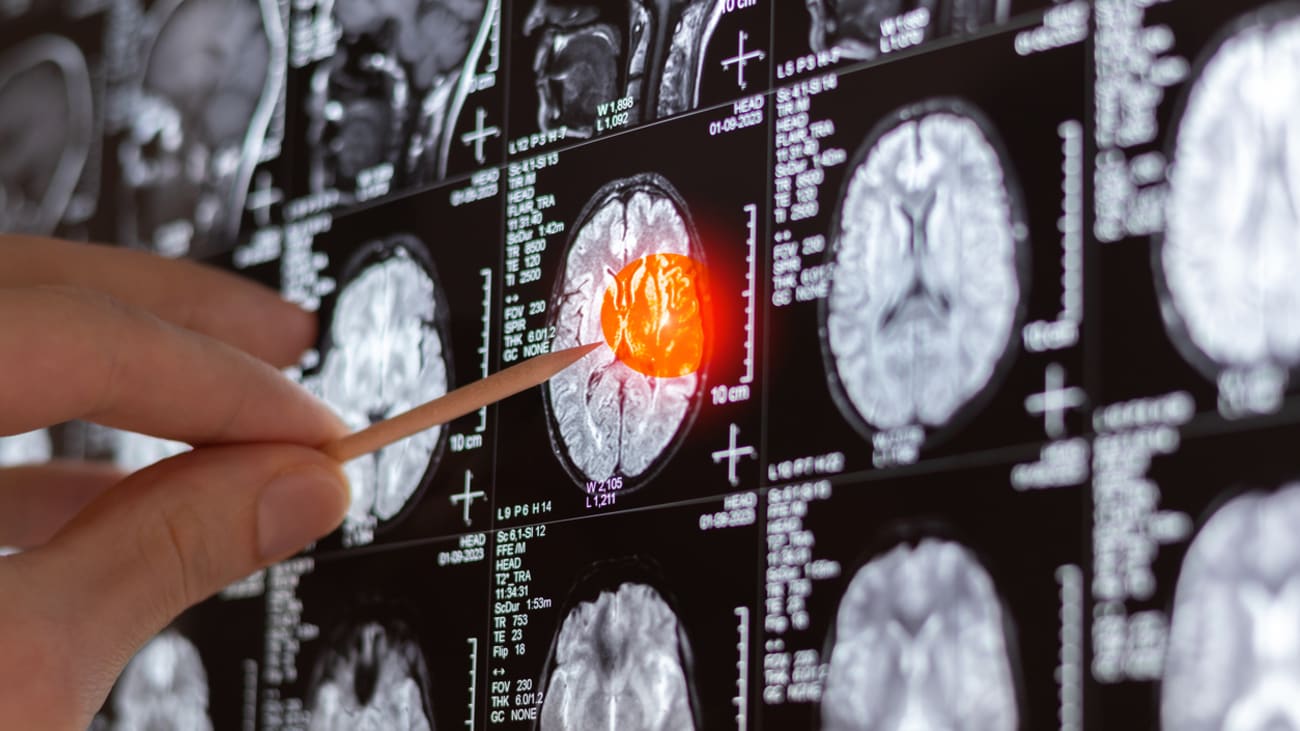
Physician-investigators at Baptist Health Miami Cancer Institute are leading groundbreaking research in the field of radiation oncology. Recently, they published five significant studies in the Journal of Neuro-Oncology and the International Journal of Radiation Oncology, Biology, Physics, revealing promising outcomes with novel approaches to treating brain tumors, including glioblastoma, and metastatic lesions in critical organs.
“Our research is having an important impact on patients,” says Rupesh Kotecha, M.D., chief of radiosurgery and director of the Central Nervous System Metastasis Program at the Institute. Along with others at the Institute, he is pioneering approaches using advanced technologies. “These publications represent our commitment to developing evidence-based protocols that optimize treatment outcomes while minimizing toxicity.”
The studies most recently published include:
- Temporospatial Tumor Dynamic Changes in Glioblastoma During Radiotherapy (Journal of Neuro-Oncology). The study showed that using MR-guided radiation therapy allows real-time visualization of tumor dynamic changes during chemoradiation and provided crucial data for developing adaptive treatment protocols that respond to these changes.
- Integrating a Novel Tablet-Based Digital Neurocognitive Assessment Tool in Brain Metastases Patients (Journal of Neuro-Oncology). The investigator-initiated trial showed that a simple, digital multi-language test used by the Institute is able to evaluate neurocognitive function among brain metastasis patients. Of approximately 200 patients who participated, 94% said the test was easy to understand, 96% found it straightforward and 74% perceived direct relevance to their care. “In the past, this was a pen-and-paper test that took hours to administer and a special team that included psychological professionals,” Dr. Kotecha says. “It was only available in English and French, which was a problem for many of our patients whose first language is Spanish, so we tested a Spanish version as well. This is an investigator-initiated trial, and we partnered with BrainLab to test the software.”
- Stereotactic Magnetic Resonance Guided Adaptive Radiation Therapy in One Fraction: A Multicenter, Single-Arm, Phase 2 Trial (International Journal of Radiation Oncology, Biology, Physics) revealed that it is feasible, safe and effective to deliver one session, called a fraction, of stereotactic body radiation therapy to a tumor using MR-guided radiation therapy. The study looked at patients with primary or metastatic lesions of the lung, liver, pancreas, adrenal gland, kidney and abdominal/pelvic lymph nodes. Local control rates at 12 months exceeded 90% for most anatomical sides, with minimal grade ?3 toxicity.
- Stereotactic Magnetic Resonance Guided Adaptive Radiation Therapy for Infradiaphragmatic Oligometastatic Disease: Disrupting the One-Size-Fits-All Paradigm (International Journal of Radiation Oncology, Biology, Physics) showed that customized radiation approaches with MR-guided radiation therapy for patients with a small number of metastatic tumors in such organs as the liver, kidney and pancreas can lead to better long-term tumor control and minimal treatment-related toxicity.
- Contrast-Enhancing Lesions Induced by Central Nervous System-Directed Intensity Modulated Proton Therapy: Distribution Patterns, Kinetics, Risk Factors, and Outcomes (International Journal of Radiation Oncology, Biology, Physics) studied the side effects of intensity modulated proton therapy, a different form of energy than traditional photon radiation. Risk increased with age, tumor volume and location, and new information is helping doctors better spare nearby tissues. This will be useful for treatment planning with proton therapy in the future.
Other Institute physician contributors include Minesh Mehta, M.D., deputy director, chief of radiation oncology and the John and Mary Lou Dasburg Endowed Chair in Radiation Oncology; and Michael Chuong, M.D., medical director of radiation oncology.
“Our comprehensive radiation therapy capabilities, with every radiation therapy modality in one setting, coupled with our robust research program, enables us to offer personalized treatment strategies, translating to improved outcomes with complex and challenging malignancies,” Dr. Kotecha says.

