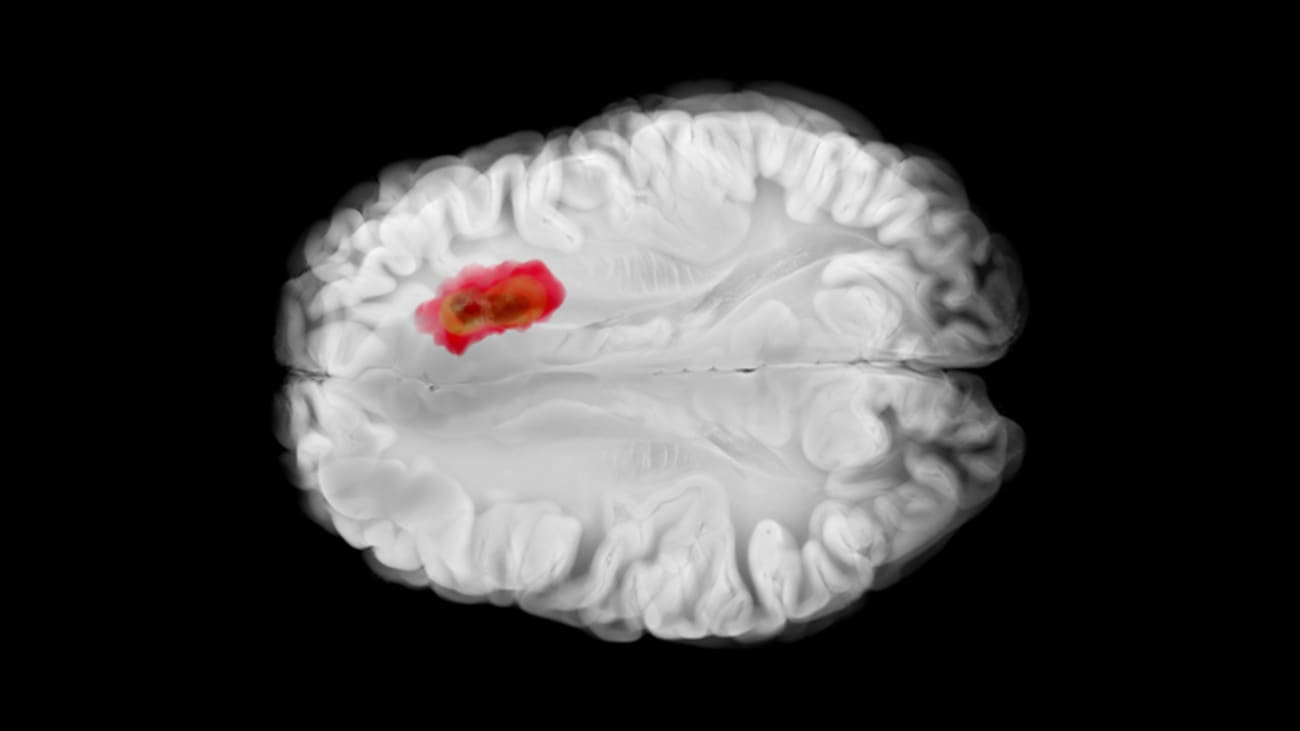

Glioma surgery in eloquent brain regions remains one of the greatest challenges in neurosurgery, demanding a balance between oncologic control and preservation of function. A recent study led by Evan Bander, M.D., Director of Endoscopic Skull Base Surgery and Co-Director of the Pituitary Tumor Program at Baptist Health Miami Neuroscience Institute, offers important new insights into how tumor location, extension, and surgical approach influence early neurocognitive outcomes after awake insular glioma resection. Beyond the publication itself, the work underscores the sophisticated array of techniques now being used at Baptist Health to maximize safety and precision in surgery for complex brain tumors.

Evan Bander, M.D.
The study examined 53 patients with insular gliomas who underwent awake craniotomy, most through a transsylvian approach and the remainder through a transcortical corridor. Neuropsychological testing before and after surgery revealed that early declines in memory and verbal fluency were common, highlighting the vulnerability of insular networks. While the overall difference between approaches was modest, patients undergoing transcortical surgery were significantly more likely to experience deterioration in verbal fluency. Tumor extension and location within the insula also mattered: left-hemisphere tumors were linked to greater declines in about half of the tested domains, lesions extending beyond the insula carried higher risk for fluency decline, and anterior or inferior quadrant tumors showed domain-specific vulnerabilities in executive function and recognition memory.
“Neurocognitive decline is common in the early term after resection of insular glioma, even when surgery is technically successful,” said Dr. Bander. “What our findings show is that these outcomes are not random, they are influenced by tumor anatomy and the pathways we use to reach them. That is critical information for both surgical planning and patient counseling.”
At Baptist Health Miami Neuroscience Institute, advanced techniques are being deployed to refine this planning process and mitigate risk. Awake craniotomy, used routinely in these cases, allows the surgical team to interact directly with the patient during tumor removal, monitoring speech, movement, and other functions in real time. “Awake mapping is an incredibly powerful tool,” Dr. Bander explained. “It allows us to resect as much tumor as possible while preserving the functions that matter most to patients. It requires a highly coordinated team – neuroanesthesia, speech and motor mapping specialists, and neuropsychologists – to make it safe and effective.”
Preoperative planning has also advanced significantly in recent years. Transcranial magnetic stimulation (TMS) is being used for noninvasive mapping of motor and speech areas before surgery. Combined with detailed neuropsychological and neurocognitive evaluations, TMS provides surgeons with a more complete picture of the functional landscape of each patient’s brain. “We now have the ability to simulate how a patient’s brain will respond to stimulation before we ever enter the operating room,” said Dr. Bander. “That level of preparation helps us choose the optimal surgical corridor and anticipate risks.”
Another innovation being integrated at Baptist Health is quicktome, a platform that leverages connectomics, to map out patient-specific connectivity profiles. By visualizing how critical language and cognitive networks are organized around a tumor, surgeons can better predict which regions are most at risk during resection. “Connectomics is changing the way we think about brain surgery,” Dr. Bander noted. “Rather than looking only at structural anatomy, we are looking at how the brain’s networks are wired in that individual. That perspective can guide both surgical decision-making and postoperative rehabilitation.”
Taken together, these technologies represent a paradigm shift toward personalized brain surgery, in which each step – from preoperative planning to intraoperative monitoring and postoperative assessment – is designed around the patient’s unique functional anatomy. The recent study serves as evidence of how these approaches yield actionable insights. It shows that outcomes after insular glioma resection are not dictated by chance but are systematically related to approach, laterality, extension, and zonal anatomy. Integrating advanced mapping and network analysis into routine practice allows the surgical team to anticipate and manage those risks proactively.
“Ultimately, our goal is to push the boundaries of safe tumor resection,” Dr. Bander said. “We want to give patients the best oncologic outcome possible, but never at the expense of their ability to think, communicate, and live independently. By combining awake surgery, intraoperative mapping, TMS, neurocognitive testing, and now connectomics, we can come closer to that ideal balance.”
The work also highlights the central role of multidisciplinary collaboration. Neuropsychologists, anesthesiologists, speech-language pathologists, radiologists, and specialized OR nurses all contribute to the awake surgery process. Baptist Health’s integrated team approach ensures that patients are supported throughout their journey, from initial evaluation through rehabilitation. “These surgeries are only possible because of the expertise and coordination of the entire team,” Dr. Bander emphasized. “It’s not just the surgeon, it’s the collective effort that makes these complex procedures safe and successful.”
As Baptist Health continues to expand its neurosurgical capabilities, the integration of research into clinical practice remains a key priority. The insular glioma study is one example of how clinical data, rigorous analysis, and advanced technology converge to improve outcomes. Future directions will include incorporating longitudinal neurocognitive follow-up, refining connectomic modeling, and developing predictive tools that combine anatomical, cognitive, and network-based risk factors.
For patients and families facing the uncertainty of brain tumor surgery, these advances provide reason for confidence. Each innovation – from awake mapping to preoperative TMS to connectome-guided planning – represents a step toward safer surgery and better preserved quality of life. For surgeons and neuroscientists, they reaffirm the value of pairing meticulous technique with cutting-edge science. And for Dr. Bander and his colleagues at Baptist Health Miami Neuroscience Institute, they reflect a commitment to delivering the most advanced, patient-centered care available today.

