
Analysis shows lower local failure with MRI-guided online adaptive treatment, supporting further prospective evaluation
A multi-institutional study led by researchers at Miami Cancer Institute, part of Baptist Health Cancer Care, and published in Cancers, offers the first direct comparison of ablative five-fraction stereotactic magnetic resonance-guided online adaptive radiation therapy (SMART) and 15/25-fraction computed tomography-guided hypofractionated ablative radiation therapy (HART) for patients with locally advanced pancreatic cancer. Conducted together with Memorial Sloan Kettering Cancer Center, the research provides clinically relevant insights into technology selection for dose-escalated radiotherapy in this challenging disease setting.

Michael D. Chuong, M.D
“While both SMART and HART achieved favorable oncologic outcomes with minimal toxicity, the significantly lower local failure observed with SMART, even in patients with more challenging tumor anatomy, suggests potential technical advantages of MR-guided online adaptive treatment,” said Michael D. Chuong, M.D., vice chair and medical director in the Department of Radiation Oncology and corresponding author of the study.
The retrospective cohort included 211 consecutive patients treated between 2016 and 2023 – 91 with SMART at Miami Cancer Institute and 120 with HART at Memorial Sloan Kettering. All patients had histologically confirmed locally advanced pancreatic cancer and had not undergone surgery. Despite a higher proportion of anatomically unfavorable tumors in the SMART cohort, including more head-of-pancreas primaries and closer proximity to gastrointestinal organs at risk, SMART achieved higher gross tumor volume coverage and greater hotspot intensities.
Two-year local failure rates were markedly lower with SMART (6.5%) compared to HART (32.9%; p < 0.001), while two-year overall survival was similar (31.0% vs. 35.3%; p = 0.056). Multivariate analysis identified treatment technique (HART vs. SMART) and induction chemotherapy regimen (non-mFOLFIRINOX vs. mFOLFIRINOX) as independent predictors of local failure. A >40% decline in CA19-9 following induction was independently associated with improved overall survival. Acute grade ?3 toxicity was low in both groups (3.3% vs. 5.8%), with late grade ?3 events less common after SMART (2.2% vs. 9.2%; p = 0.037).
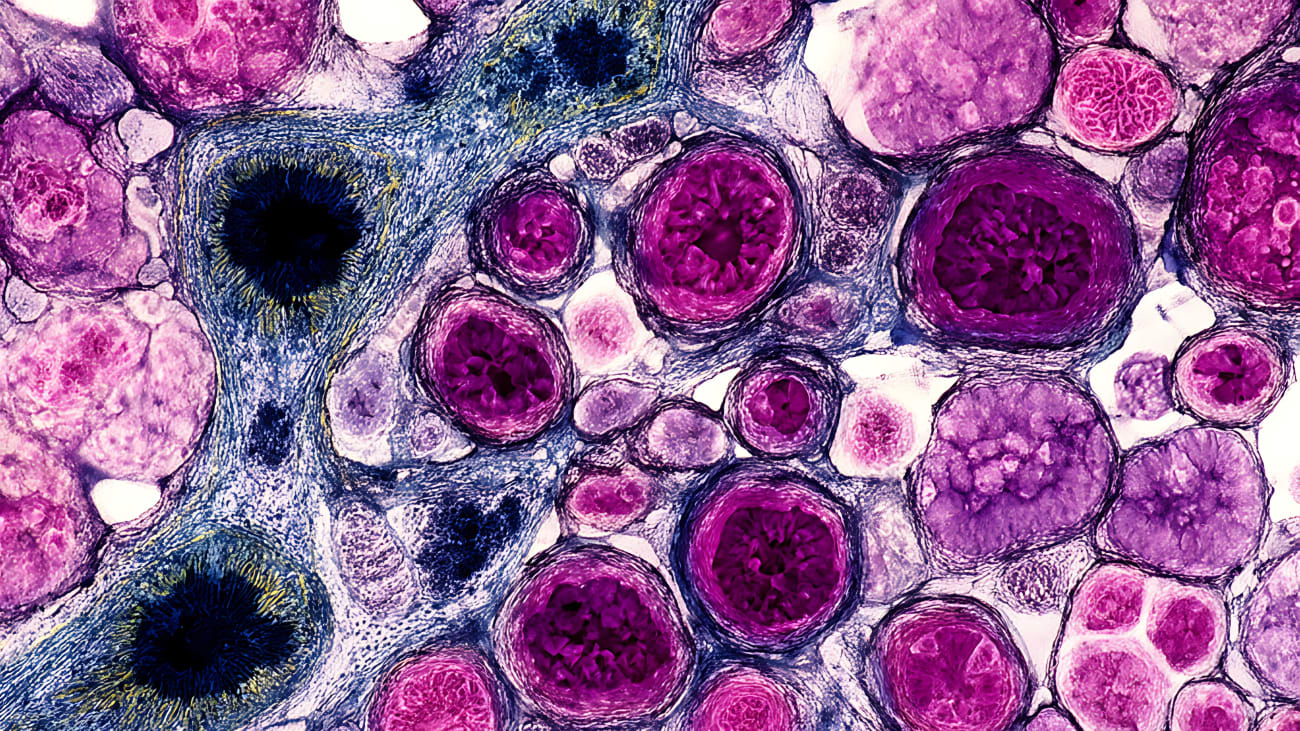
The investigators emphasize that daily online adaptive replanning with SMART may have facilitated improved target coverage and allowed for more permissive hotspot dosing without exceeding gastrointestinal organ-at-risk constraints. These capabilities, combined with large fraction sizes of ?10 Gy, may enhance indirect tumor cell kill through mechanisms such as endothelial apoptosis and vascular injury.
Dr. Chuong added, “Our findings are hypothesis-generating and support the need for prospective trials to determine whether the improved local control with SMART can translate into an overall survival benefit. Given the limited availability of MR-Linac platforms, HART remains an important and effective option at centers with advanced motion management capabilities on conventional linear accelerators.”
The study adds to a growing body of evidence supporting ablative dose escalation for locally advanced pancreatic cancer, with both techniques achieving outcomes superior to historical controls treated with chemotherapy with or without non-ablative radiation. As clinical trial networks such as NRG Oncology move forward with randomized evaluations of dose-escalated regimens, including elective coverage, these results provide important guidance for technology and protocol selection in high-volume pancreatic cancer programs.
To learn more about Dr. Chuong and his work, please click here.

