
New research connects changes in brain networks after radiotherapy to declines in memory and cognition.
Advances in medical imaging and neuroscience have made it possible to look at the human brain in increasingly sophisticated ways. One such development is “connectomics,” the study of how different parts of the brain are connected and work together. A new proof-of-concept study, conducted by a team at Baptist Health South Florida, published in Cancers, looked at how whole-brain radiotherapy (WBRT), a common treatment for patients with brain metastases, affects these brain connections, and how the resulting changes might be linked to declines in thinking and memory skills.

Rupesh Kotecha, M.D..
The study focused on 10 patients with brain metastases who were treated with WBRT. Brain metastases are cancerous tumors that spread to the brain from other parts of the body, such as the lungs or breast. “WBRT is often used to treat patients with numerous brain tumors, but is known to carry the risk of causing cognitive problems,” said Rupesh Kotecha, M.D., chief of radiosurgery, director of central nervous system metastasis at Miami Cancer Institute, and senior author of the study. “We wanted to understand if these cognitive side effects could be linked to changes in the brain’s ‘connectome,’ the intricate web of neural connections that support mental functioning.”
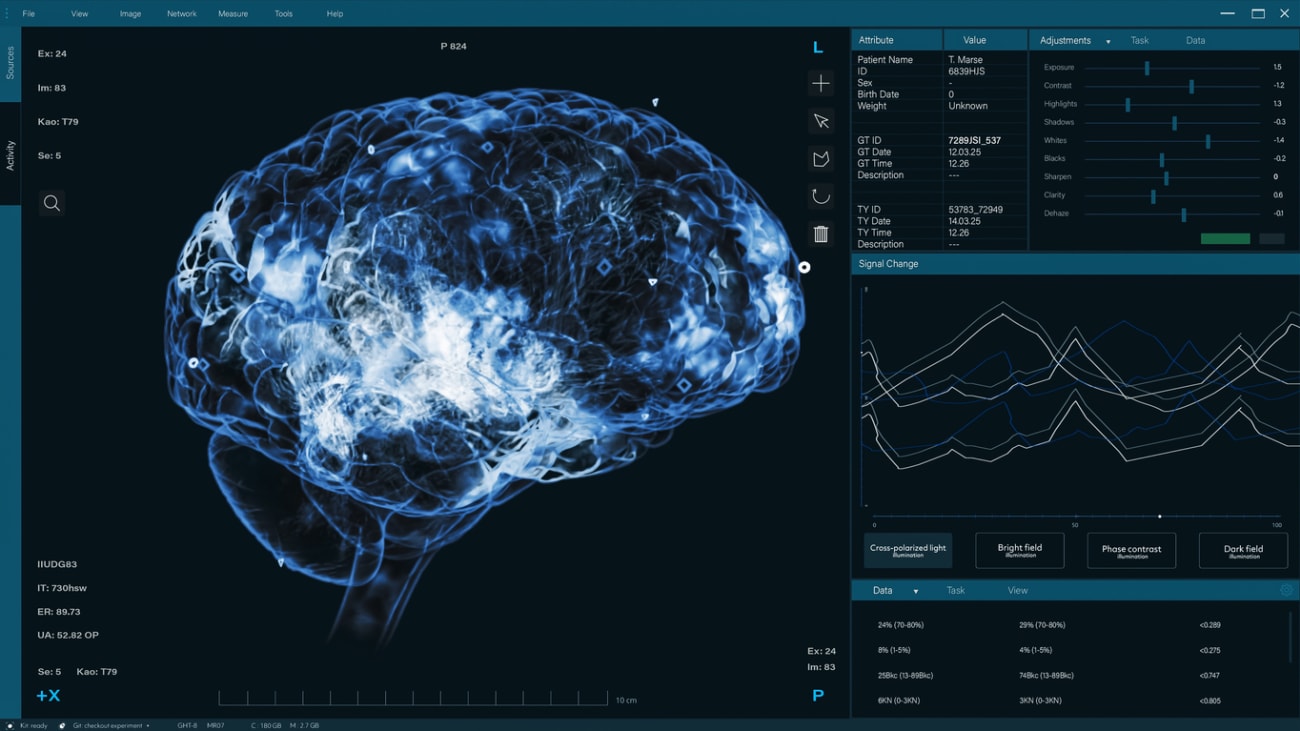
To investigate this, the Baptist Health team of researchers used two advanced brain imaging methods: diffusion tensor imaging, which shows the brain’s structural wiring, and functional MRI, which maps out active brain areas when at rest. They applied machine learning techniques to create personalized brain maps for each patient, highlighting 15 key brain networks involved in functions like memory, attention, and motor control.
These brain maps were compared to those from healthy individuals in a large brain mapping project called the Human Connectome Project. By identifying areas of unusually high or low activity, the researchers could assess how WBRT impacted the brain’s functional networks.

Michael W. McDermott, M.D.
Before receiving WBRT, patients already showed numerous anomalies, likely due to the presence of cancer and previous treatments like surgery or focused radiation. On average, each patient had about 10 affected brain networks. The networks with the most abnormalities were those responsible for high-level thinking and decision-making; specifically, the multiple demand network (which supports tasks like working memory and problem-solving), the paralimbic network (involved in emotional processing), and the central executive network.
“Three months after WBRT, imaging showed that the number and severity of anomalies increased in most patients,” said Michael W. McDermott, M.D., chief medical executive, Irma and Kalman Bass Endowed Chair in Clinical Neuroscience at Baptist Health Miami Neuroscience Institute, and co-author of the publication. “On average, 12 of the 15 networks were now affected, with the limbic network and the paralimbic network showing the greatest increases in abnormal activity. In contrast, some networks, like those involved in basic sensory processing and vision, actually showed fewer anomalies.”
The researchers also performed neurocognitive assessments using a novel tablet-based app that measured several domains of thinking, including memory, attention, motor skills, and verbal fluency. These tests were administered before treatment and again three months later. Among the patients who completed both assessments, many showed declines in memory-related tasks, especially in recalling and recognizing words.
Most strikingly, the study found a strong correlation between declines in memory function and changes in a specific brain network – the subcortical network. This network includes deep brain structures like the thalamus, basal ganglia, and hippocampus, which are essential for memory, attention, and learning. Patients whose subcortical networks showed more anomalies were more likely to experience memory decline. Conversely, patients treated with a specialized form of WBRT that spares the hippocampus – a key memory center – showed fewer such changes, suggesting that sparing critical regions might help preserve cognitive function.
“These findings add to growing evidence that WBRT can significantly alter brain connectivity and that these changes may underlie the cognitive side effects many patients report after treatment,” said Starlie Belnap, director of Baptist Health Brain & Spine Care Research and Outcomes, and co-author of the study. “Our findings also support the idea that imaging the brain’s connectome could become a valuable tool in planning and adapting treatments to reduce long-term side effects.”
While the study involved a small number of patients, it highlights the potential of connectomics to personalize cancer care. By identifying which brain networks are most vulnerable and linking those changes to specific cognitive functions, future treatments might be better tailored to each patient. For example, radiation doses could be adjusted to minimize damage to key networks, or supportive therapies could be introduced to protect or rehabilitate cognitive function.
In conclusion, this study shows that brain mapping using connectomics can reveal important insights into how treatments like WBRT impact brain function. It also underscores the importance of considering not just the physical control of cancer, but also the quality of life and cognitive health of survivors. As technology continues to evolve, integrating connectome data into clinical decision-making could represent the next frontier in personalized, brain-sparing cancer therapy.

